In Vitro Fertilisation IVF is a treatment for fertility where the ovaries are stimulated to produce an increased number of eggs, these eggs are then are put together with sperm in the laboratory where they fertilise to form an embryo. When developed to an appropriate stage the embryo is transferred back into the uterus where implantation takes place. The process of IVF is undertaken in the following stages:
Ovarian Stimulation The growth of ovarian follicles is controlled by hormones from the pituitary gland at the base of the brain. Normally only enough hormone is produced to allow one follicle to grow to full maturity. The medication used to stimulate the ovaries is recombinant follicle stimulating hormone (Puregon® or Gonal-F®). These medications promote the growth of several follicles so that the number of oocytes obtained is increased.
The current stimulation options utilised in IVF treatment include:
GnRH antagonist (short cycle) The stimulation phase of your treatment cycle commences on day 2 after the beginning of your period.
An antagonist drug (Orgalutran® or Cetrotide®) is commenced on the 5th or 6th day after FSH injections. This switches off the pituitary gland’s control of ovulation. The time from commencement of treatment to pregnancy test is approximately 4 weeks.
Down Regulation with Synarel® Synarel® is used in the pre-treatment cycle to switch of the pituitary gland’s control of ovulation. This enables the developing follicles to be synchronised under the influence of the follicle stimulation hormone injections.
Synarel® is a nasal spray and is used morning and night. It is continued until the time of your oocyte retrieval. The stimulation phase of the treatment cycle can begin after your period commences and you have ‘baseline’ hormone levels. The time from commencement of treatment to pregnancy test is approximately 6 weeks.
Down Regulation with the oral contraceptive pill and Synarel The oral contraceptive pill and Synarel® are used in the pre-treatment cycle to switch off the pituitary gland’s control of ovulation. This enables the developing follicles to be synchronised under the influence of the follicle stimulation hormone injections.
Synarel® is a nasal spray and is used morning and night. It is continued until the time of your oocyte retrieval. The stimulation phase of the treatment cycle can begin after your period commences and you have ‘baseline’ hormone levels. The time from commencement of treatment to pregnancy test is approximately 8 weeks.
Flare Tubal problems Synarel® or Lucrin® commences on day 2 of your period, and continues until the time of your oocyte retrieval. The stimulation stage commences within a few days of starting the Synarel® or Lucrin®.
Monitoring As the follicles grow they produce the hormone oestrogen which can be measured in the blood. Therefore blood tests tell us how your ovaries are responding to treatment and allow us to modify treatment where necessary.
The number of follicles and their size will also be measured by ultrasound. Sound waves are used to assess the size of each growing follicles in the ovary. The scan is performed using a probe inserted into the vagina. This procedure requires an empty bladder. Partners are welcome to be present during scans. You may have several scans during a treatment cycle.
Blood tests and ultrasounds are usually planned to commence approximately 9 days after starting the FSH injections and the combined results are used to decide the ideal time for oocyte retrieval.
There are no restrictions to having sexual intercourse during the stimulation phase of the treatment cycle. Sexual intercourse or ejaculation is recommended the evening prior to the first ultrasound.
Trigger When the follicles reach the appropriate size the time for oocyte retrieval will be decided and you will give an injection of Ovidrel® in the evening at a time advised by the clinic. Ovidrel® acts to complete the maturation (ripening) of the oocytes within the follicles and to initiate changes in the follicle which lead to ovulation. This injection is timed so that the oocyte retrieval occurs approximately 34-36 hours later.
Egg Pick Up The usual method of collecting eggs is via ultrasound guided vaginal oocyte retrieval. This is performed in the operating theatre at St Andrew’s Hospital as a day procedure. Usually a light anaesthetic will be administered by an anaesthetist, although you may choose to have this performed under local anaesthetic.
The ultrasound probe is placed in the vagina with the tip against the vaginal wall. The ovaries are usually positioned near the other side of this wall and are readily visualised. Under ultrasound guidance a needle is passed through the vaginal wall and into the ovarian follicles which are then drained of fluid.
The follicular fluid is collected into a test tube and then transferred into a dish. The contents are examined under a microscope to determine whether an oocyte has been recovered. An oocyte is not always obtained from each follicle.
This procedure takes about 20-30 minutes, depending on the number of follicles to be drained. You will need to stay in hospital for a minimum of 2 hours following your oocyte retrieval and should not drive for 24 hours. It is recommended that you have someone stay with you overnight.
Semen Collection Following the oocyte retrieval, the male partner is requested to produce a semen specimen by masturbation. The nursing staff will have informed you of the time your partner will be required. A short delay for the semen collection is of no concern, as we have allowed enough time if there is a problem collecting the specimen.
A minimum of 2 days and not more than 7 days abstinence from sexual intercourse and ejaculation is recommended prior to oocyte retrieval. If you feel that there may be problems producing a sample on request, please discuss this with us prior to commencing treatment. In some circumstances, pre-treatment semen samples may be frozen as a ‘back up’. Occasionally a semen sample may contain insufficient motile sperm to fertilise an oocyte. If this happens, the male partner may be requested to produce a second specimen later that same day.
In some situations surgical sperm retrieval will be required. Your doctor will discuss this with you if necessary. A fact sheet is available with further information on these procedures and will be provided if required in your particular situation.
Embryo Development and Fertilisation Washed sperm will be added to the eggs or the washed eggs injected (see ICSI below) with a sperm a few hours after the egg collection. The eggs and sperm will then be placed in an incubator overnight.
18-24 hours after the sperm and eggs are placed together the scientist will inspect the eggs to establish whether fertilisation has occurred. On average 70% of eggs will fertilise. The presence of a pronuleus indicates normal fertilisation has occurred.
Different culture media are used for different stages of embryo development. The culture medium is a fluid that contains all the nutrients and essential components to support fertilisation and development of the embryo during its culture period in the lab, prior to transfer back to the uterus or freezing.
Embryo Transfer The date of embryo transfer will be determined according to the length of time the embryo has been allowed to develop i.e. cleavage stage or blastocyst. The embryo transfer is done as an outpatient procedure and lasts 15 minutes. The procedure does not require an anaesthetic. Your partner is welcome to be present during this procedure. You will be required to lie on the bed with your legs supported to allow positioning of a speculum to visualise the cervix (similar to the procedure for a pap smear). The embryo is drawn into a fine plastic tube (catheter) attached to a small syringe. The catheter is passed through the cervix and the embryos placed back inside the uterus. If more than one embryo is to be transferred they are both placed in the same catheter. The catheter is then checked to ensure that the embryos have been released into the uterus.
You may have the opportunity to view your embryos on a TV monitor prior to their transfer.
After the procedure, we advise that you resume your normal healthy lifestyle. We suggest you limit strenuous physical activity and avoid becoming overheated eg. Saunas, spas, sunbathing. You may resume sexual intercourse at any time following embryo transfer.
Luteal Phase Management Following the embryo transfer you will be start progesterone pessaries or Crinone Progesterone vaginal gel Occasional Pregnyl (hCG) may be used - this decision is determined by your hormone levels These injections, which are given once or twice, stimulate the production of the hormone progesterone, which maintains the inner lining of the uterus, the endometrium.
During this time you may experience abdominal cramping, abdominal distension, sore breasts and ovarian tenderness. If you have any concerns please contact the nursing staff. A pregnancy test will be performed approximately 18 days after your egg pick up. If your period commences it is important to contact the nursing staff in the clinic.
IVF
In Vitro Fertilisation
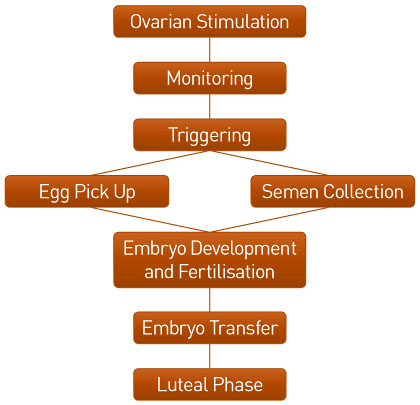
IVF is a treatment for fertility where the ovaries are stimulated to produce an increased number of eggs, these eggs are then are put together with sperm in the laboratory where they fertilise to form an embryo. When developed to an appropriate stage the embryo is transferred back into the uterus where implantation takes place. The process of IVF is undertaken in the following stages:
Ovarian Stimulation
The growth of ovarian follicles is controlled by hormones from the pituitary gland at the base of the brain. Normally only enough hormone is produced to allow one follicle to grow to full maturity. The medication used to stimulate the ovaries is recombinant follicle stimulating hormone (Puregon® or Gonal-F®). These medications promote the growth of several follicles so that the number of oocytes obtained is increased.
The current stimulation options utilised in IVF treatment include:
GnRH antagonist (short cycle)
The stimulation phase of your treatment cycle commences on day 2 after the beginning of your period.
An antagonist drug (Orgalutran® or Cetrotide®) is commenced on the 5th or 6th day after FSH injections. This switches off the pituitary gland’s control of ovulation. The time from commencement of treatment to pregnancy test is approximately 4 weeks.
Down Regulation with Synarel®
Synarel® is used in the pre-treatment cycle to switch of the pituitary gland’s control of ovulation. This enables the developing follicles to be synchronised under the influence of the follicle stimulation hormone injections.
Synarel® is a nasal spray and is used morning and night. It is continued until the time of your oocyte retrieval. The stimulation phase of the treatment cycle can begin after your period commences and you have ‘baseline’ hormone levels. The time from commencement of treatment to pregnancy test is approximately 6 weeks.
Down Regulation with the oral contraceptive pill and Synarel
The oral contraceptive pill and Synarel® are used in the pre-treatment cycle to switch off the pituitary gland’s control of ovulation. This enables the developing follicles to be synchronised under the influence of the follicle stimulation hormone injections.
Synarel® is a nasal spray and is used morning and night. It is continued until the time of your oocyte retrieval. The stimulation phase of the treatment cycle can begin after your period commences and you have ‘baseline’ hormone levels. The time from commencement of treatment to pregnancy test is approximately 8 weeks.
Flare
Tubal problems Synarel® or Lucrin® commences on day 2 of your period, and continues until the time of your oocyte retrieval. The stimulation stage commences within a few days of starting the Synarel® or Lucrin®.
Monitoring
As the follicles grow they produce the hormone oestrogen which can be measured in the blood. Therefore blood tests tell us how your ovaries are responding to treatment and allow us to modify treatment where necessary.
The number of follicles and their size will also be measured by ultrasound. Sound waves are used to assess the size of each growing follicles in the ovary. The scan is performed using a probe inserted into the vagina. This procedure requires an empty bladder. Partners are welcome to be present during scans. You may have several scans during a treatment cycle.
Blood tests and ultrasounds are usually planned to commence approximately 9 days after starting the FSH injections and the combined results are used to decide the ideal time for oocyte retrieval.
There are no restrictions to having sexual intercourse during the stimulation phase of the treatment cycle. Sexual intercourse or ejaculation is recommended the evening prior to the first ultrasound.
Trigger
When the follicles reach the appropriate size the time for oocyte retrieval will be decided and you will give an injection of Ovidrel® in the evening at a time advised by the clinic. Ovidrel® acts to complete the maturation (ripening) of the oocytes within the follicles and to initiate changes in the follicle which lead to ovulation. This injection is timed so that the oocyte retrieval occurs approximately 34-36 hours later.
Egg Pick Up
The usual method of collecting eggs is via ultrasound guided vaginal oocyte retrieval. This is performed in the operating theatre at St Andrew’s Hospital as a day procedure. Usually a light anaesthetic will be administered by an anaesthetist, although you may choose to have this performed under local anaesthetic.
The ultrasound probe is placed in the vagina with the tip against the vaginal wall. The ovaries are usually positioned near the other side of this wall and are readily visualised. Under ultrasound guidance a needle is passed through the vaginal wall and into the ovarian follicles which are then drained of fluid.
The follicular fluid is collected into a test tube and then transferred into a dish. The contents are examined under a microscope to determine whether an oocyte has been recovered. An oocyte is not always obtained from each follicle.
This procedure takes about 20-30 minutes, depending on the number of follicles to be drained. You will need to stay in hospital for a minimum of 2 hours following your oocyte retrieval and should not drive for 24 hours. It is recommended that you have someone stay with you overnight.
Semen Collection
Following the oocyte retrieval, the male partner is requested to produce a semen specimen by masturbation. The nursing staff will have informed you of the time your partner will be required. A short delay for the semen collection is of no concern, as we have allowed enough time if there is a problem collecting the specimen.
A minimum of 2 days and not more than 7 days abstinence from sexual intercourse and ejaculation is recommended prior to oocyte retrieval. If you feel that there may be problems producing a sample on request, please discuss this with us prior to commencing treatment. In some circumstances, pre-treatment semen samples may be frozen as a ‘back up’. Occasionally a semen sample may contain insufficient motile sperm to fertilise an oocyte. If this happens, the male partner may be requested to produce a second specimen later that same day.
In some situations surgical sperm retrieval will be required. Your doctor will discuss this with you if necessary. A fact sheet is available with further information on these procedures and will be provided if required in your particular situation.
Embryo Development and Fertilisation
Washed sperm will be added to the eggs or the washed eggs injected (see ICSI below) with a sperm a few hours after the egg collection. The eggs and sperm will then be placed in an incubator overnight.
18-24 hours after the sperm and eggs are placed together the scientist will inspect the eggs to establish whether fertilisation has occurred. On average 70% of eggs will fertilise. The presence of a pronuleus indicates normal fertilisation has occurred.
Different culture media are used for different stages of embryo development. The culture medium is a fluid that contains all the nutrients and essential components to support fertilisation and development of the embryo during its culture period in the lab, prior to transfer back to the uterus or freezing.
Embryo Transfer
The date of embryo transfer will be determined according to the length of time the embryo has been allowed to develop i.e. cleavage stage or blastocyst. The embryo transfer is done as an outpatient procedure and lasts 15 minutes. The procedure does not require an anaesthetic. Your partner is welcome to be present during this procedure. You will be required to lie on the bed with your legs supported to allow positioning of a speculum to visualise the cervix (similar to the procedure for a pap smear). The embryo is drawn into a fine plastic tube (catheter) attached to a small syringe. The catheter is passed through the cervix and the embryos placed back inside the uterus. If more than one embryo is to be transferred they are both placed in the same catheter. The catheter is then checked to ensure that the embryos have been released into the uterus.
You may have the opportunity to view your embryos on a TV monitor prior to their transfer.
After the procedure, we advise that you resume your normal healthy lifestyle. We suggest you limit strenuous physical activity and avoid becoming overheated eg. Saunas, spas, sunbathing. You may resume sexual intercourse at any time following embryo transfer.
Luteal Phase Management
Following the embryo transfer you will be start progesterone pessaries or Crinone Progesterone vaginal gel Occasional Pregnyl (hCG) may be used - this decision is determined by your hormone levels These injections, which are given once or twice, stimulate the production of the hormone progesterone, which maintains the inner lining of the uterus, the endometrium.
During this time you may experience abdominal cramping, abdominal distension, sore breasts and ovarian tenderness. If you have any concerns please contact the nursing staff. A pregnancy test will be performed approximately 18 days after your egg pick up. If your period commences it is important to contact the nursing staff in the clinic.